
Case Study #1 At Home Therapy System for Neuropathic Pain
Integrum AB, a prosthetics company located in Gothenburg, Sweden has developed Neuromotus ®, a new therapy system for patients with neuropathic pain, specifically Phantom Limb Pain which is experienced by a majority of people who have lost a limb. The therapy encourages Phantom Motor Execution, an exercise that works through reactivating the original central and peripheral circuitry involved in motor control of missing limbs, and increases dexterity of muscles at the stump in hopes of inducing gradual neural changes in the motor cortex.
Neuromotus ® is currently undergoing CE marking by Integrum AB as well as a large clinical trial throughout Europe following a clinical trail with results published in multiple journals including the medical journal The Lancet. I was approached by the company which I had worked with during my research fellowship year to design the system for At Home Use.
The System

The virtual reality driven therapy system uses pattern recognition from recorded surface electromyography (sEMG) muscle signals. The patient is asked to perform a movement (flex wrist, extend wrist etc.) of the missing limb and the muscle signals are recorded. Pattern recognition algorithms are used to classify each movement. The information is then fed to a virtual arm, that is superimposed on the patient using a fiducial marker to mark the position of the phantom limb in the augmented reality. Additionally the processed sEMG data can act as a control for gaming and virtual reality.

The Challenge
Currently the device is designed for clinical use therefore the next step for this therapy is to take the technology out of the clinic and redesign for the patient to perform the therapy at home. However, the move from lab use to home use presents usability challenges that must first be addressed through User Centered Design in order to ensure safe and effective therapy for the patient.
The Impact
Phantom Limb Pain is often experienced as a shooting, stabbing ,squeezing , throbbing or burning pain that comes from the lost limb (outside the residual limb) and can negatively impact the quality of life of those who suffer from it, especially when it distracts and interferes with work, sleep, and the activities of daily life. This often leads patients to rely on varying forms of pain medications and opioids just to sleep through the night. Adapting the therapy to the home environment increases accessibility of the treatment and provides a drug free alternative to pain treatment. The therapy at home allows the patients to follow the therapy regime when they need it the most. In short, it gives the patient independence and autonomy over their health and wellness.

At-Home Research Team on the road to patients´ homes in Sweden
Left- Shannon Brown (Me) UX Designer, Usability and User Researcher
Driver- Allie Middleton, PhD Student in Medical Anthropology, Princeton University
Backseat- Eva Lendaro, PhD Student in Biomedical Engineering ,Chalmers University of Technology
My Role
The investigation was performed September 2017 - December 2018 for my master thesis work in the program of Interaction Design at Chalmers University of Technology in Gothenburg, Sweden. I worked under the direction of Dr. Max Ortiz Catalán at the Biomechatronics and Neurorehabilitation Lab with a team of researchers focusing on the use of novel human computer interfaces (including Neuromotus) in the home environment. This team traveled around Sweden to collect both qualitative and quantitative data from the patients who were given the technology to use at home. This home study and development was done in partnership with product developers and engineers at Integrum AB.
My role in the project was to perform a usability analysis of the device and to design and collected survey data, perform short interviews relating to use patterns in order to inform design of the User Interface, UX and interaction design elements of the digital interface. Below outlines a few of my contributions to the project as a UX Researcher.

The Approach
The development process followed the User Centered Design Methodology following the IEC 62366 (2007) and FDA Guidelines (2010) which describe the User Centered Design Process for Usability Testing in Medical Devices. These standards were used primarily to analyze the efficacy of use of the system at home.
Phase 1: Literature Review

Understanding Patient Motivation
For a holistic understanding of the wider challenges facing patients who perform physical therapy at home, a thorough literature review was performed. I quickly learned that in the field of physical therapy that patient motivation was one of the strongest predictor of success for a therapy regime. In addition, studies have found that with outpatient care the majority of patients do not follow the prescribed therapy regime because they were unwilling or unable to fit the therapy into their daily life.

Designing for Motivation
In searching through the literature I found a framework for designing for at-home physiotherapy patients to support their motivation¹ . There are six elements that support patient motivation at home. I decided to prioritize four of them: Understanding, Enjoyment, Results and Scheduling. These four elements are more within the patients` control when doing the therapy. I did not include the external motivational factors of a support and peer network.
Phase 2: User Research

Surveys, Ethnographic Study and Observations
1. Surveys - used to understand general usage and attitudes towards the current clinical device from clinicians, as well as the 4 patients who utilize the device at home.
2. Ethnographic Studies - Visited the patients at home to understand context of use and gain a better understanding of their use patterns and attitudes towards the therapy system. Visits provided insight on how individuals understand, troubleshoot and set up the therapy. Performed short interviews in Swedish and English with patients and caretakers.
3. Observations - Observed at home patients using the current system as well as patients and clinicians using the current system in the clinic during the clinical trial
Phase 3: Synthesizing Insights
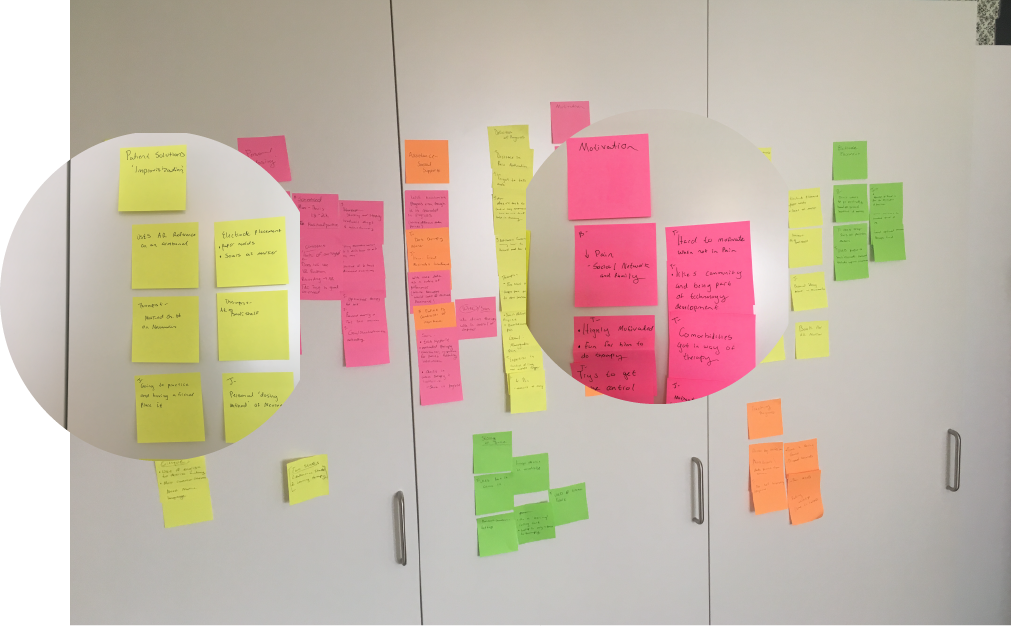
KJ Analysis
An affinity diagram was created from the ethnography study which consisted of the both interviews, observations, and the user surveys regarding the use of the Neuromotus ® at home and in the clinic to organize the disparate ideas and observations of each patient into user needs.

User Personas and Journey
User personas were developed as a design tool from the User Research phase to reflect user types and map out how they would use the device in relevant contexts. Personas helped to understand user characteristics, needs and goals. I created two main patient personas: one who uses the device based on time while the other uses the device based on achieving a specific goal. I used these personas to map a User Journey and identify user pain points. Pain points included the system set up time, unclear goal markers for the goal-oriented user, and the troubleshooting of poor or unusable sEMG signals.
Phase 4: Defining Functionalities

Functional Diagraming
After I better understood the context of use with the above phases, the user requirements were decided upon and a functional diagram was created to identify how the system contributes to accomplishing the user’s intent.
Phase 5: Ideation
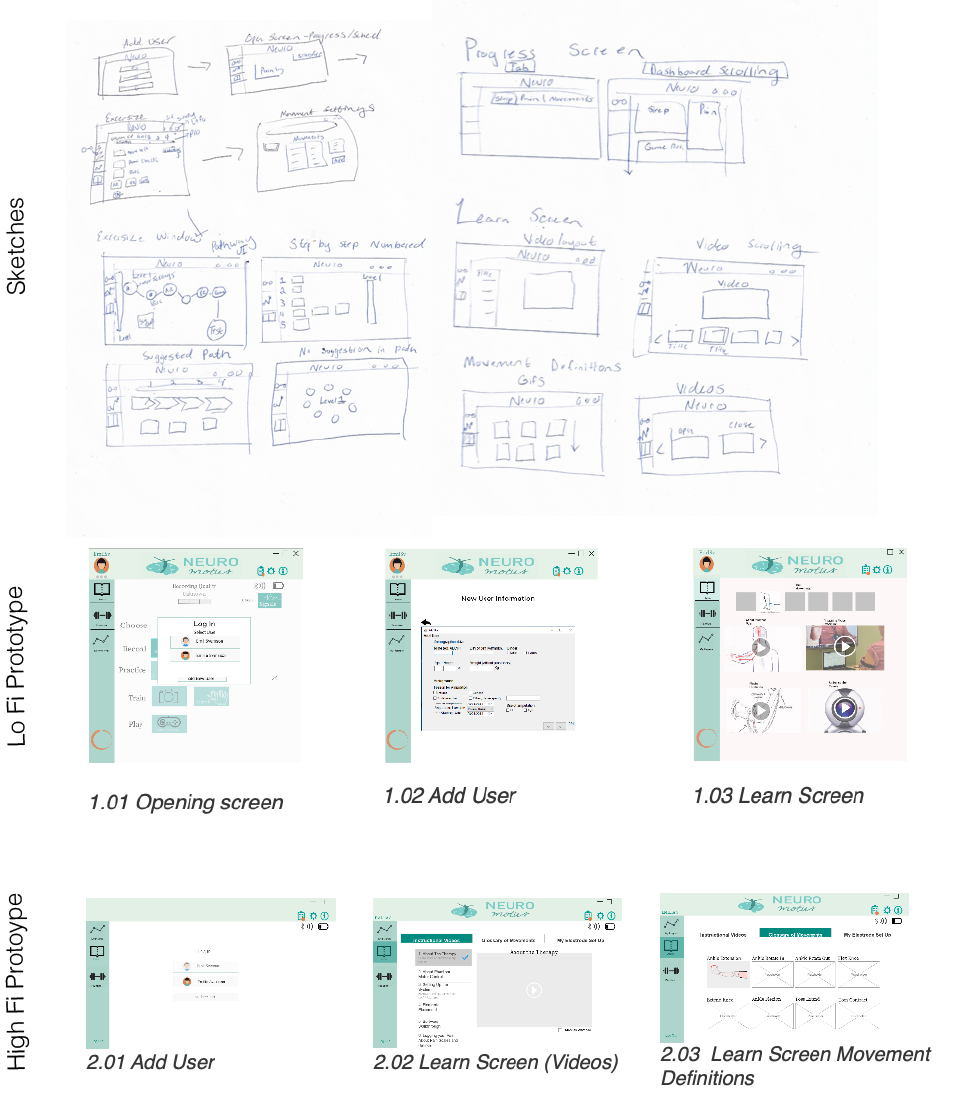
User Interface Design and Testing
Low Fidelity Sketches - Used to brainstorm ideas for a new user interfaces that address the key functionalities
Lo Fi Prototype - Used for formative evaluation with development team to test logic in navigation schemes and location of content
High Fi Prototype - Clickable interface used for remote user test with Patient who currently uses the system at home
Phase 6: Final Proposal

The proposal was delivered to engineers and developers at Integrum AB with a style guide, html link, user flow charts, and a usability analysis.
The proposed interface for at-home use attempts to address patient motivation using the attributes found in literature review and patient feedback to increase motivation including designing for understanding, enjoyment, results and scheduling. The product is ready to undergo verification and field testing.

1. Motivation by Understanding
In order to increase user understanding a “learn” section was added to the user interface (UI) that includes videos about the therapy, movement definitions, and a log for how the patients set up the electrodes to record a therapy session. Another addition to the UI in the practice interface was an indicator that shows the user the level of intensity of their exercise.

2. Motivation by Enjoyment
With the addition of the movement rewards, the therapy was gamified for more enjoyment. Although the rewards may not make the exercises themselves more enjoyable the reward tokens aim to provide clear and immediate feedback based on movement accuracy measurements. For example, top scores in the race car game and consecutive exercise streaks are logged to encourage time spent in the therapy. In this way the patient can directly see their progression in the therapy and therefore feel less frustrated with the lengthy time it may take to see progress.

3. Motivation by Results
In the survey participants reported difficulty in understanding their progress through their long-term therapy at home. Therefore, the interface contains a progress screen in which the user can review their pain log (a result of the pain survey) which includes a graph showing their weekly pain and overall pain pattern. A log in which the user could input their pain medication intake was also included. The pain medication intake window was added as a result of the user test in which the user reported the decrease in pain medication intake as one of the primary markers of success. The patient’s ability to explore charts and graphs of their historical performance and subjective reports of pain enables them to gain a wider perspective on their treatment progress

4. Motivation by Scheduling
Another reason for not adhering to the therapy regime is forgetting to do the exercise. Patients report difficulty in trying to regularly integrate the therapy in their lives because the sessions currently take 1-2 hours. In order to enable self-sufficiency, a calendar section was added to the interface that allows the patient to set their own training schedule. The schedule should give a suggestion about the duration and frequency of the therapy, but permits personalization and change of plans. Push notifications and calendar integration are also features to help remind patients of their own goal-setting.
Publications
Lendaro E, Middleton A, Brown S, Ortiz-catalan M. Out of the Clinic , into the Home : The in-Home Use of Phantom Motor Execution Aided by Machine Learning and Augmented Reality for the Treatment of Phantom Limb Pain. J Pain Res. 2020;Volume 13:195-209. doi:10.2147/JPR.S220160.
Works Cited
1. H. Chandra, I. Oakley, and H. Silva, “Designing to support prescribed home exercises: understanding the needs of physiotherapy patients,” in Proceedings of the 7th Nordic Conference on Human-Computer Interaction: Making Sense Through Design, 2012, pp. 607–616.
Reflections
I chose this thesis work so that I could thoroughly go through a product development cycle following IEC and FDA guidelines in Usability Engineering for medical devices within the context of a meaningful application. During the course of the thesis year I worked closely with other researchers in engineering and anthropology, as well as stakeholders including clinicians and patients to thoroughly understand the implications and design requirements of providing a neuropathic pain therapy at home. I also had the opportunity to continue to work with a group of talented big hearted researchers and developers who work on the cutting edge of Human Machine Interface Design to improve the lives of amputees and those with motor impairments around the world and delve deeper in my understanding of the science behind the work completed at the Biomechatronics and Neurorehabilitation lab.
This project is part of a collaborative effort between Chalmers researchers, BNL and Integrum AB in order to develop technologies to restore quality of life after traumatic events leading to amputations or motor impairments. This multidisciplinary team works with biomedical instrumentation, bioelectric signals processing, machine learning and human-machine interfaces. Learn more about our work and ongoing projects on the BNL Facebook Page linked below

